
MRI-guided brain surgery easier on Parkinson’s patients
Published March 25, 2013
Since 2002, more than 70,000 patients have undergone deep brain stimulation (DBS) surgery to treat their symptoms.
Yet, the brain surgery is about eight hours long and difficult for patients, who have to be awake through some of the operation. Not only that, but Parkinson’s patients have to go off their medications before the surgery, often causing them much pain and discomfort.
“The thought of being awake and having brain surgery is stressful for patients,” said Dr. Hooman Azmi, director of the division of movement disorders at Hackensack University Medical Center in New Jersey. “I’ve had patients who are just so worried about it that they don’t want the surgery or there are patients that just never go to surgeons because of these fears."
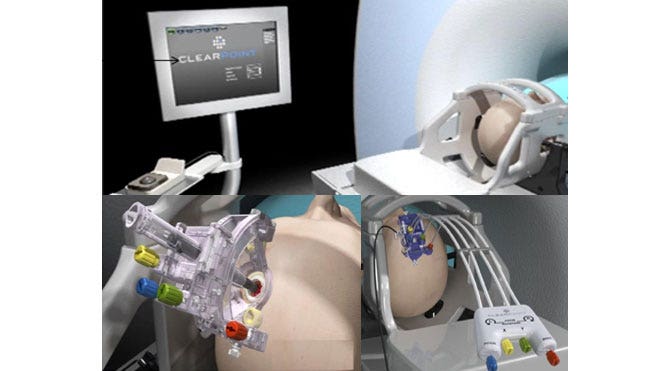
Over the last two years, brain surgeons have begun using a new computer-driven surgical system to reduce these drawbacks of the surgery and to improve the accuracy of the procedure. The new system, called ClearPoint, uses magnetic resonance imaging (MRI) during the surgery (it’s done in the MRI suite, not the OR) to precisely pinpoint the target for the pacemaker in real time.
Traditionally, the surgery is done through a small burr hole and is based on images taken before surgery and “stereotactic” techniques, which provide a 3-D coordinate system and brain mapping to help hit the target as precisely as possible. A “lead” or thin, insulated wire is implanted in the brain and the tip of the wire is within the targeted area, which is about the size of a pea (the battery pack is typically implanted under the skin near the collarbone).
“The benefits of the surgery depend on how accurately we place it, and the side effects depend on our accuracy as well,” Azmi said.
Because the brain can shift ever so slightly, surgeons need the patient’s feedback from the electrical activity of the brain to be sure they’ve hit their target—that’s why patients need to be woken up during the surgery. The operation can take eight hours because it requires extensive brain mapping and waking the patient out of their anesthesia. The reason patients have to go off their medications is because the drugs mask the symptoms. Surgeons need patients to experience the symptoms in order to tell if the DBS wire is accurately positioned to reduce them.
With ClearPoint, the surgeon uses MRI images taken during surgery to visualize the brain and see the precise target during the surgery. Because of this precision, there’s no need to wake the patient during surgery and patients can stay on their medications because the surgeon no longer needs to “test” whether they’ve hit their target. The procedure takes about half the time.
“Surgery is safer because it’s shorter; the patient is more comfortable, (and) we can see the wires going in," Azmi said. "If there’s any bleeding we could see it."
The system, which is being used in 18 medical centers in the U.S., can also be used to treat other movement disorders treated by DBS such as essential tremors and dystonia, which causes muscle contractions.
http://www.foxnews.com/health/2013/03/25/mri-guided-brain-surgery-easier-on-parkinsons-patients/

No comments:
Post a Comment