Julian Keenan of Montclair State University’s Biology and Psychology departments talks about research and how parts of the brain can be turned off to prevent lying.
Julian Keenan of Montclair State University’s Biology and Psychology departments speaks with Montclair Patch about his research about lying. Montclair State University
Whether you are young or old, everyone tells lies in one way or another on a daily basis.
Of course, there are all sorts of different lies — white lies, exaggerations, delusions, deceptions — and some are worse than others. But regardless of the what kind of lie it is, the same parts of the brain are used in manufacturing the fabrication.
As April Fool’s Day approaches, Montclair Patch decided to talk with professor Julian Keenan of Montclair State University’s Biology and Psychology departments about the science of lies.
A portion of the conversation is below.
What kind of research have you done on the topic of lying?
Keenan: We are looking at what areas of the brain are involved in deception, and the lying we are most interested in is the lying people do to themselves or what goes on in your brain when you are telling yourself that you are better than you are, smarter than you are, funnier than you are.
So you can see specific parts of the brain becoming active when someone is telling a lie?
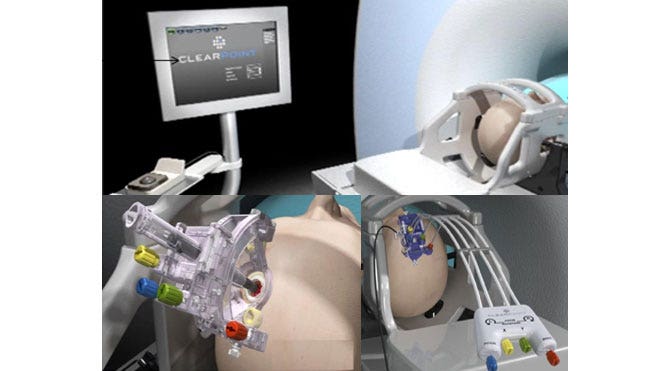
Keenan: Yes, but unfortunately the brain works like that for a lot of different things. So at Montclair State, we use a machine called transcranial magnetic stimulation, or TMS, which is able to block certain types of the brain from functioning for a brief amount of time — a fraction of a second.
So we ask people questions and ask them to lie. If we are focusing on the right part of the brain using TMS, they won’t be able to lie.
How then do you turn those parts of the brain off?
Keenan: This is the part where people really become interested.
The TMS machine is placed up against the skull and you can target a part of the brain as small as 1 centimeter by 1 centimeter. It turns off parts of the brain by creating a magnetic field and makes all the cells in that small area of the brain work at once. When all the cells work at once, they don’t work at all, which creates a virtual lesion.
The uses for TMS seem ideal for interrogations and intelligence gathering, no?
Keenan: I could care less about that stuff, but yes, some people are using TMS for interrogation purposes.
Is the technology being used widely by law enforcement?
Keenan: It is being used widely. The problem is that it is not reliable enough, and not immiscible in court.
What else have you found in your research about lying?
Keenan: People love to tell themselves lies. We found what people throughout time have found: People lie to themselves all the time. The brain is not very concerned with reality; the brain is concerned about making you feel better.
Is it natural for us to lie then?
Keenan: Absolutely. Lying is healthy and a sign of high intelligence.
Kids are lying by the age of 2. And while 2-year-olds are horrible liars, kids usually begin lying well enough to get away with it by the age of 5.
Is lying tied to self-esteem then?
Keenan: Yes. The more we lie to ourselves, the better we feel.
People with clinical depression are more based in reality than people without depression, because they see the world as it really is by lying to themselves less.
http://maplewood.patch.com/articles/msu-professor-on-lies-and-the-human-brain